Full Service Denials Management
About Us
Our mission is to provide the most effective, efficient and timely denial-recovery service in the market.
We are driven by integrity, transparency, responsibility, and accountability. What we say is what we do. Guaranteed.
- We use only U.S.-based physicians with expertise in inpatient medical-necessity and coding denials to write our appeals. Our physicians are actively practicing at large hospitals in the United States. This ensures our physicians are clinically up-to-date and have a true understanding of the inpatient admission decision making process.
- Our physicians receive ongoing education and training for appeal writing. They are well versed in the appeals process, including state and federal regulations, nationally accepted clinical criteria, and the tactics that insurance companies use to deny payments to health care institutions.
- Our physicians receive ongoing education and training for appeal writing. They are well versed in the appeals process, including state and federal regulations, nationally accepted clinical criteria, and the tactics that insurance companies use to deny payments to health care institutions.
- Technology underpins all that we do. It speeds our work and assures our accuracy. Our online web portal lets clients access everything in their accounts, anytime. Moreover, our secure technology allows our team of physicians to work remotely to fit their own schedules. This leads to improved efficiency, speed, appeals success, and accelerated cash flow for our clients.
- Our proprietary methods reverse denials at the industry’s highest rate: 78%.
- We have a proven track record of recovering maximum revenue for our clients.
- We routinely provide clients with tools and insights to prevent and fight new denials.
Why Us
Centralized Appeals, LLC was founded in 2014 by Daniel Schreier, a highly experienced medical-necessity appeals expert. Dan has designed our unique propriety process and personally oversees all that we do.
We do not stop appealing denied claims until either victory or total exhaustion of your appeal rights. Using expert physicians to write appeals, and a tenacious staff to manage them on our proprietary denials software application, we routinely boost our clients’ revenues.
We combine people, process, and cutting-edge technology to provide the industry’s most effective, cost-efficient, and timely approach. Our speed fuels our success. And we share our knowledge with our clients, so they can improve their internal denial management skills.
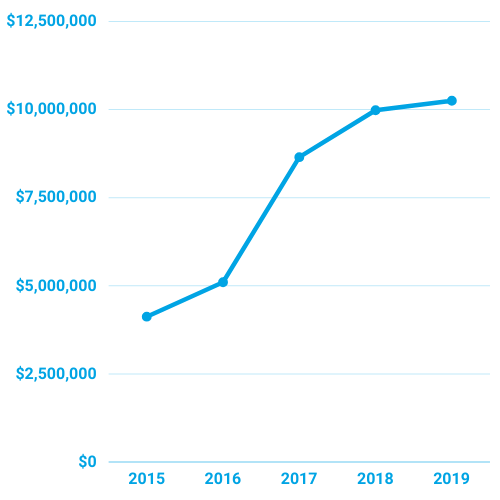
Our high success rate (78% successful appeals) provides our clients a consistent source of monthly revenue. We frequently hear from our clients that CA’s returns have made it far easier to pay their bills. Since 2015, CA has collected more than $35,000,000 for our clients. In 2019, CA overturned 58% of 1st level appeals resulting in cash collections of $8,000,000 for our clients. Of the upheld first level appeals, CA overturned 35% of External Appeals resulting in additional cash collections of $1,000,000 for our clients.
Losing appeals never will cost you money! We only invoice for revenue that we collect, which is on a 100% contingency basis. We never will bill for unsuccessful appeal efforts. Hence our motto: Our success is measured by your success. Partnering with Centralized Appeals on your denial management efforts is risk-free.
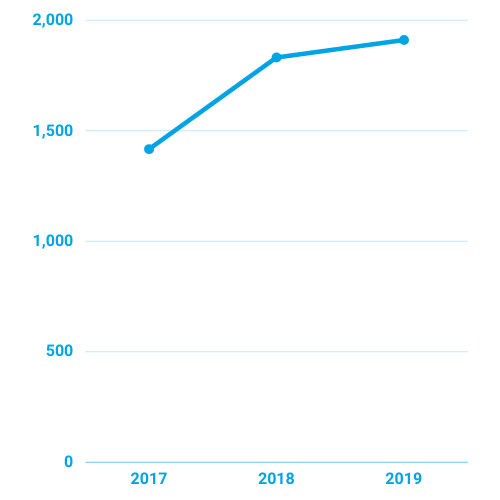
Appeals Volume
Client's Revenue
The Team
We have a team of over 30 Appeals Physicians. Our appeals-writing doctors are:
- All U.S. based and currently between ages 30 and 45.
- Actively practicing at well-known hospitals across America.
- Graduates of well-known U.S. medical schools.
- Extremely technology enabled.
- Exceptional writers.
Daniel Schreier
Chief Executive Officer & Founder
Benjamin Schreier
Chief Technology Officer
The Process
CA’s Clock starts from receipt of the denial referral from the denial liaison.
- CA receives denial referral from denial liaison.
- CA enters the denial file and associated data (e.g. due date, payer, patient name, expected reimbursement, admitting physician, financial class, admit/discharge date, etc.) into our database.
- CA requests the medical records from the Health Information Management (HIM) department. For denials, the medical record can immediately be downloaded from Epic.
- Denial file is assigned and submitted to a physician appeal writer to write the appeal. For administrative denials, the denial file is assigned to an administrative appeals expert.
- Physician appeal writer completes the appeal and our software platform notifies CA’s clerical team that the appeal was completed and ready for submission to payer.
- CA submits the appeal to the payer
- Payer issues acknowledgement letter that the appeal was received, which CA notes in the Health Information System (HIS)/Patient Accounting System.
- CA will follow-up to confirm appeal receipt, where applicable.
- Appeal decision is made by the payer.
- Appeal Decision letter is issued to member hospital.
- CA will request the decision letter and upload into the HIS, where applicable.
- CA documents the appeal outcome in our internal database as well as HIS/Patient Accounting System.
- CA will enter claim payments for approved appeals into our database.
- CA will run daily aging reports from our database which we will use to follow-up with the payers for unpaid claims with approved appeals. Payers have 45 days from the appeal approval date to pay claims timely per New York State’s Prompt Pay Laws regulation. In the event a payment was made but never posted to the Patient Accounting System, CA will submit a request along with the pertinent details/documentation to the respective cash poster for resolution.
- For upheld denials/first level appeal losses, CA will file external appeals or second level appeals, where applicable. If the appeal rights are exhausted, CA will submit a request via email to a designated contact to downgrade or write off the denial account.
- For upheld denials with missing external appeal medical record release consent forms, CA will pursue the missing forms from the patient. We will pursue the required forms until we receive them or the external appeal rights expire
- External appeal is approved or upheld.
- CA will enter claim payments for approved appeals into our database.
- CA will follow-up with payers for untimely claim payments for approved external appeals.
- CA will file complaints with Provider Representatives and subsequently regulators if necessary.
- For upheld external appeals/cases with exhausted appeal rights, CA will submit a request via email to a designated contact to downgrade or write off the denial account.
Our Technology...
- Self-Service/Knowledge Transfer: you can easily access your data at anytime, anywhere.
- Live insight: Real time analytics into denials and appeals activity including:
- Denials and Appeals Data aggregation by year with data including root cause of denials, revenue collected, revenue pending, top denying payer, top denied admitting physician, and inability to file appeals.
- Provide targeted education for denials reduction and improved clinical documentation.
- Learn about problems with managed care contracts.
- Convenience: CA’s Appeals Physician can work remotely anytime, anywhere. No special hardware if required.
- Clinically Driven Appeals: Our software is a repository for all clinical literature and nationally accepted clinical criteria for inpatient admission, which is updated periodically.
- User friendly interface: Our interface allows the Appeals Physician to request a new Denial File, move easily from screen to screen (e.g. from the medical record to the appeal letter to the clinical literature/guidelines), and submit the appeal file as completed.
- One Stop Shop for Everything: the software application can be accessed anywhere at any time.
- Repository for Medical Records, Appeal Letters, Remittance Documents, etc.
- New denials are entered into the software application with all the relevant datapoints (including the appeal due date) and we mark them under the status ready for assignment. Subsequently, the Denial Files will become available in the Appeals Physician available inventory, which means the Appeals Physician can click “Request a Denial File” which will assign a Denial File to the requesting Appeals Physician. The system automatically assigns the Denial File to the Appeals Physicians by due date, meaning the most urgently due appeals are assigned first.
- Matching Appeal Needs with Clinical Expertise: For certain specialty cases requiring specific expertise, we can manually assign a denial file to an Appeals Physician with a correlating specialty (i.e. a cardiology case with a cardiologist, pediatric with pediatrician, etc.).
- Realtime Appeal Monitoring: CA’s software has reports with sorting and filtering to see exactly what stage the appeal is in and the next course of action. Examples include:
- Run a report of all first level appeals without a determination and sort by age. Next step follow-up with the payers for appeal status
- Run a report of all denials without an appeal submission and submit the appeal.
- Run a report for all appeal approvals without a claim payment and sort it by age. We then can follow-up with the payer for claim payment status/next steps for overdue unpaid claims with approved appeals.
Our Software:
- Cuts the appeals-process time by up to 50%, rapidly accelerating clients’ cash flow.
- Allows clients to log into CA’s web portal and see real-time snapshot of their denials and appeals activity.
- Is highly scalable for growing our physician-appeal writer base and maximizes the efficiency/volume of our physician-appeal writers.
- Captures every data-point associated with denials and appeals.
Contact us today!
Centralized Appeals will perform an assessment of your inpatient claims write offs for the past six months, to identify opportunities to increase revenue.
Phone: 917-704-3632
Fax: 516-534-2050
Email: Info@CentralizedAppeals.com
Address: P.O. Box 1622 New York, NY 10028
Centralized Appeals is Fully Insured with General Liability, Cyber Liability, & Professional Liability Insurance.
© 2026 Centralized Appeals.
